Difference between revisions of "SNAP and Other Federal Nutrition Programs"
(changing vague word (evidence), fixing double-word error ('which which'), addition of a paragraph in the "Decision Power" section) |
(Fixing the formatting of my added references to match the rest.) |
||
| Line 25: | Line 25: | ||
</ref> O'Neil says math is demonstrated to be not only entangled in the world’s problems, but also fueling them, <ref name=CathyONeil></ref> and this math determines which individuals qualify for social benefits. Numbers such as income and assets can be the difference between “food insecure” and food security. | </ref> O'Neil says math is demonstrated to be not only entangled in the world’s problems, but also fueling them, <ref name=CathyONeil></ref> and this math determines which individuals qualify for social benefits. Numbers such as income and assets can be the difference between “food insecure” and food security. | ||
| − | When algorithms, like the mass algorithm used in SNAP, do not take into account possible biases by the humans who wrote them, the biases can have lasting effects. A study done by Obermeyer et al. found that commercial algorithms used by the U.S healthcare system continuously concluded that black patients were healthier than white patients. <ref name=health>Obermeyer, Z., Powers, B., Vogeli, C., & Mullainathan, S. (2019, October 25). [https://science.sciencemag.org/content/366/6464/447.abstract?casa_token=vatDAfV8NDMAAAAA%3ANHUxKrKQj5v2Xc-4hUiMpZGC7hml7BBKIs5RaC5cPdDK8OpjkFxOTFNuj5lXGGohjHe2KTXUSKWhtEo “Dissecting racial bias in an algorithm used to manage the health of populations.”] </ref> | + | When algorithms, like the mass algorithm used in SNAP, do not take into account possible biases by the humans who wrote them, the biases can have lasting effects. A study done by Obermeyer et al. found that commercial algorithms used by the U.S healthcare system continuously concluded that black patients were healthier than white patients. <ref name=health>Obermeyer, Z., Powers, B., Vogeli, C., & Mullainathan, S. (2019, October 25). [https://science.sciencemag.org/content/366/6464/447.abstract?casa_token=vatDAfV8NDMAAAAA%3ANHUxKrKQj5v2Xc-4hUiMpZGC7hml7BBKIs5RaC5cPdDK8OpjkFxOTFNuj5lXGGohjHe2KTXUSKWhtEo “Dissecting racial bias in an algorithm used to manage the health of populations.”]. ScienceMag.org. </ref> |
The algorithm was inherently incorrect because it used health costs as a proxy for health needs, and less money is spent on black patients with the same need. <ref name=health> </ref> Context of the actual situation sometimes needs to be utilized instead of trusting an algorithm’s outcomes. With SNAP, individuals and families who are on the border are concluded as food secure when that is not the case. <ref name=gingold></ref> | The algorithm was inherently incorrect because it used health costs as a proxy for health needs, and less money is spent on black patients with the same need. <ref name=health> </ref> Context of the actual situation sometimes needs to be utilized instead of trusting an algorithm’s outcomes. With SNAP, individuals and families who are on the border are concluded as food secure when that is not the case. <ref name=gingold></ref> | ||
| Line 36: | Line 36: | ||
===Cost of Food Insecurity=== | ===Cost of Food Insecurity=== | ||
[[File:ebott_snap2.png|400px|right|thumb|Graphs highlighting food insecure individual's medical costs by state. <ref name=cdc2> Berkowitz SA, Basu S, Gundersen C, Seligman HK. [State-Level and County-Level Estimates of Health Care Costs Associated with Food Insecurity. Prev Chronic Dis 2019;16:180549. DOI: http://dx.doi.org/10.5888/pcd16.180549 </ref>]] | [[File:ebott_snap2.png|400px|right|thumb|Graphs highlighting food insecure individual's medical costs by state. <ref name=cdc2> Berkowitz SA, Basu S, Gundersen C, Seligman HK. [State-Level and County-Level Estimates of Health Care Costs Associated with Food Insecurity. Prev Chronic Dis 2019;16:180549. DOI: http://dx.doi.org/10.5888/pcd16.180549 </ref>]] | ||
| − | The failure to meet SNAP's qualifications leads to an increase in healthcare expenses for the left-out individuals on the border. In a longitudinal cohort study, the researchers showed that being food insecure was associated with significantly more emergency room visits, hospitalizations, and days hospitalized. <ref name=ncbi>Berkowitz, S., Seligman, H., Meigs, J., & Basu, S. (2018, September 10). [https://www.ajmc.com/view/food-insecurity-healthcare-utilization-and-high-cost-a-longitudinal-cohort-study “Food insecurity, healthcare utilization, and high cost: A longitudinal cohort study”]. </ref> The average cost of an emergency room visit in 2017 was $1,389. <ref name=cost>(Nov. 12, 2020).[ https://www.debt.org/medical/emergency-room-urgent-care-costs/ “Emergency room vs. urgent care: Differences, costs & options”]</ref> That price can be lower with insurance, but with high deductibles, the individual would still have to pay the full price if they haven’t reached their deductible. <ref name=ded>Hunt, Janet. (Mar. 03, 2021). [https://www.thebalance.com/average-cost-of-an-er-visit-4176166#citation-2 “Average Cost of an ER Visit”]</ref> With these added costs, individuals who are food insecure had annual health care expenses that were $1834 higher than individuals who are food secure. The total median annual health care cost for food insecure individuals was $687,041,000. <ref name=cdc2> Berkowitz SA, Basu S, Gundersen C, Seligman HK. [State-Level and County-Level Estimates of Health Care Costs Associated with Food Insecurity. Prev Chronic Dis 2019;16:180549. DOI: http://dx.doi.org/10.5888/pcd16.180549 </ref>. | + | The failure to meet SNAP's qualifications leads to an increase in healthcare expenses for the left-out individuals on the border. In a longitudinal cohort study, the researchers showed that being food insecure was associated with significantly more emergency room visits, hospitalizations, and days hospitalized. <ref name=ncbi>Berkowitz, S., Seligman, H., Meigs, J., & Basu, S. (2018, September 10). [https://www.ajmc.com/view/food-insecurity-healthcare-utilization-and-high-cost-a-longitudinal-cohort-study “Food insecurity, healthcare utilization, and high cost: A longitudinal cohort study”]. </ref> The average cost of an emergency room visit in 2017 was $1,389. <ref name=cost>(Nov. 12, 2020).[https://www.debt.org/medical/emergency-room-urgent-care-costs/ “Emergency room vs. urgent care: Differences, costs & options”]. Debt.org.</ref> That price can be lower with insurance, but with high deductibles, the individual would still have to pay the full price if they haven’t reached their deductible. <ref name=ded>Hunt, Janet. (Mar. 03, 2021). [https://www.thebalance.com/average-cost-of-an-er-visit-4176166#citation-2 “Average Cost of an ER Visit”]<. The Balance./ref> With these added costs, individuals who are food insecure had annual health care expenses that were $1834 higher than individuals who are food secure. The total median annual health care cost for food insecure individuals was $687,041,000. <ref name=cdc2> Berkowitz SA, Basu S, Gundersen C, Seligman HK. [State-Level and County-Level Estimates of Health Care Costs Associated with Food Insecurity. Prev Chronic Dis 2019;16:180549. DOI: http://dx.doi.org/10.5888/pcd16.180549 </ref>. |
| − | These costs add an increased strain on food insecure individuals as compared to food secure individuals and perpetuates the poverty cycle. Food insecurity is linked with poorer health outcomes, as well as higher health care costs. This cycle continues because there is a link between high health care needs and greater out-of-pocket costs and higher levels of food insecurity. <ref name=sonic> Sonik, R. A. (2019). [https://ajph.aphapublications.org/doi/full/10.2105/AJPH.2019.305252?casa_token=ayf9i7W4-t4AAAAA:dv4xRb7-MJH0a5Q6RKOwi5xvZzd9JIfLXo0A_kUUy2e56iLNY-jtA-5dHOTMXBExXagOSm5uxW_xzsQ “Health insurance and FOOD Insecurity: Sparking a Potential virtuous cycle”]. American Journal of Public Health, 109(9), 1163-1165. doi:10.2105/ajph.2019.305252 </ref> This cycle is especially difficult to break out of for children who grew up in poverty. Out of the children who experience moderate-to-high levels of poverty, 35% to 46% are also poor throughout early and middle adulthood. <ref name=pov> Wagmiller, R., & Adelman, R. (2009, November).[ https://www.nccp.org/publication/childhood-and-intergenerational-poverty/ “Childhood and intergenerational poverty: The long-term consequences of growing up poor”]. </ref> | + | These costs add an increased strain on food insecure individuals as compared to food secure individuals and perpetuates the poverty cycle. Food insecurity is linked with poorer health outcomes, as well as higher health care costs. This cycle continues because there is a link between high health care needs and greater out-of-pocket costs and higher levels of food insecurity. <ref name=sonic> Sonik, R. A. (2019). [https://ajph.aphapublications.org/doi/full/10.2105/AJPH.2019.305252?casa_token=ayf9i7W4-t4AAAAA:dv4xRb7-MJH0a5Q6RKOwi5xvZzd9JIfLXo0A_kUUy2e56iLNY-jtA-5dHOTMXBExXagOSm5uxW_xzsQ “Health insurance and FOOD Insecurity: Sparking a Potential virtuous cycle”]. American Journal of Public Health, 109(9), 1163-1165. doi:10.2105/ajph.2019.305252 </ref> This cycle is especially difficult to break out of for children who grew up in poverty. Out of the children who experience moderate-to-high levels of poverty, 35% to 46% are also poor throughout early and middle adulthood. <ref name=pov> Wagmiller, R., & Adelman, R. (2009, November).[https://www.nccp.org/publication/childhood-and-intergenerational-poverty/ “Childhood and intergenerational poverty: The long-term consequences of growing up poor”]. National Center for Children in Poverty.</ref> |
==References== | ==References== | ||
<references/> | <references/> | ||
Revision as of 17:19, 18 March 2021
One of the most prominent federal nutrition programs is the United States Department of Agriculture Supplemental Nutrition Assistance Program (SNAP), formerly known as Food Stamps, which provides monetary nutrition benefits to supplement food budgets of families in need to move towards self-sufficiency. This program reached 38 million people nationwide in 2019, of which more than 66% were in families with children; average monthly SNAP benefits for each household member ranged from $100-200 depending on location. [1] This program and other similar federal nutrition programs can be understood as an information technology because it uses a mass formula which is an algorithm that could be automated to determine individual and family eligibility.
Contents
Overview
Eligibility
The determination of eligibility follows a set of strict federal rules.[2] To be eligible for benefits, a household’s income and resources must meet three core criteria: gross monthly income must be at or below 130 percent of the poverty line, net income must be at or below the poverty line, and assets must fall below certain limits. Additionally, there are certain groups of people who are not eligible for SNAP benefits regardless of their income, including individuals on strike, unauthorized immigrants, and some lawfully present immigrants. [2] The mass formula for determining eligibility skips people that do not qualify numerically.
A Note on COVID-19
Until January 16, 2021 with the introduction of the Consolidated Appropriations Act 2021, students in college were not eligible for SNAP benefits [3] -- some eligibility rules were temporarily expanded during COVID-19, lasting until September 30, 2021. [3] This act temporarily expanded eligibility to higher education students if they meet one of two specific new criteria. [3] Prior to this change many students had to look elsewhere for food assistance.
During the pandemic, avoiding public areas such as grocery stores is important when individuals have pre-existing conditions. The United States Center for Disease Control recommends to avoid public spaces to limit risk of exposure to COVID-19. [4] Many people have to rely on grocery delivery services, and very few online grocery delivery services will accept SNAP payments. [5] This difficulty in using SNAP benefits during COVID-19 raises food security concerns for many individuals. [5]
Ethical Concerns
Failure to Meet Needs
There are many cases of individuals and families in need of food that do not qualify for SNAP based on the mass formula algorithm. More than 41 million people are "food insecure", meaning that they do not have consistent access to adequate food, and roughly 1 in 4 of these individuals are not likely to be eligible for programs such as SNAP. [6] Having these hard guidelines for eligibility means that there are some cases where individuals miss the qualification by a few dollars over the limit. [6] Additionally many individuals that are on SNAP benefits struggle to make ends meet with the small allotment decided upon. Despite the algorithm determining they have sufficient funds, NPR gives specific examples of individuals with food security struggles. [5]
Due to changes in congressional power and presidency, there are amendments made to the existing eligibility requirements. One of the more recent changes cut off an estimated 700,000 unemployed people from food assistance provided by SNAP. [7] This change targeted a group of people known as able-bodied adults without dependents. Taking support from some of those individuals can harm more than just them -- many of those people share their benefits with family or their social network and can create a ripple-effect from these cuts.
Decision Power
Bias in information systems also can exist within public services, not just private corporations. There are deep historical roots of biases against the poor that characterize today’s “tools of digital poverty management”. [8] These biases, harmful or not, are ingrained in information technologies and their corresponding algorithms. Such algorithms can have tremendous impacts on individual’s lives and the social aids they receive -- they can determine who is at risk of child abuse, who is best suited for a given job, and in this case, who is eligible for “food stamps”.
These federal nutrition programs can be thought of in context of a “weapon of math destruction”. Cathy O’Neil, coiner of this term, says that these WMDs can combine data injustice and systemic inequality to trap poor people in negative “feedback loops”. [9] O'Neil says math is demonstrated to be not only entangled in the world’s problems, but also fueling them, [9] and this math determines which individuals qualify for social benefits. Numbers such as income and assets can be the difference between “food insecure” and food security.
When algorithms, like the mass algorithm used in SNAP, do not take into account possible biases by the humans who wrote them, the biases can have lasting effects. A study done by Obermeyer et al. found that commercial algorithms used by the U.S healthcare system continuously concluded that black patients were healthier than white patients. [10] The algorithm was inherently incorrect because it used health costs as a proxy for health needs, and less money is spent on black patients with the same need. [10] Context of the actual situation sometimes needs to be utilized instead of trusting an algorithm’s outcomes. With SNAP, individuals and families who are on the border are concluded as food secure when that is not the case. [5]
Health Impacts
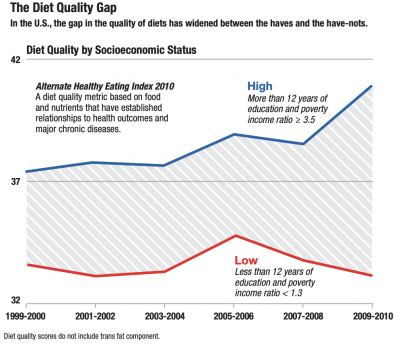
Determination from this information technology has ethical implications on the health and well-being of individuals. Failure to meet qualifications for SNAP and other federal nutrition programs means that many individuals have to make the most of their money by skipping meals, buying the cheapest (processed) foods, and not having the support to purchase more expensive fresh foods such as fruits and vegetables. [6] The current benefit maximum allotment is 115% of the June 2020 value of the Thrifty Food Plan (TFP), which is roughly $45 per week for males and $40 per week for females. [11]
A review of 27 studies in 10 countries including the United States found that unhealthy food is on average $1.50 cheaper per day than healthy food. [12] Given the relative cost of processed and “healthy” foods, it is easier to meet daily nutritional needs by spending this little amount of money on processed foods. These cheaper foods are less nutritious than the latter and can put individuals at higher risks for health problems. [12] Davis' research has shown that the Thrifty Food Plan does not consider labor cost and is thus inadequate. [13] Using a basic labor economics technique, the study determined that with labor included, the mean household falls short of the TFP health guidelines even with the determined monetary resources. [13] Children living in low-income families have worse health outcomes on average than other children on a number of indicators such as obesity and mental health. [14] These negative health correlations with poverty levels are extended from information technologies such as these federal nutrition support programs.
Cost of Food Insecurity
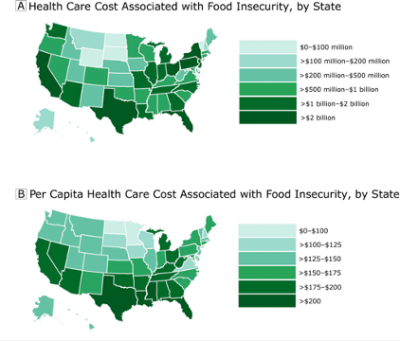
The failure to meet SNAP's qualifications leads to an increase in healthcare expenses for the left-out individuals on the border. In a longitudinal cohort study, the researchers showed that being food insecure was associated with significantly more emergency room visits, hospitalizations, and days hospitalized. [16] The average cost of an emergency room visit in 2017 was $1,389. [17] That price can be lower with insurance, but with high deductibles, the individual would still have to pay the full price if they haven’t reached their deductible. Cite error: Closing </ref> missing for <ref> tag.
These costs add an increased strain on food insecure individuals as compared to food secure individuals and perpetuates the poverty cycle. Food insecurity is linked with poorer health outcomes, as well as higher health care costs. This cycle continues because there is a link between high health care needs and greater out-of-pocket costs and higher levels of food insecurity. [18] This cycle is especially difficult to break out of for children who grew up in poverty. Out of the children who experience moderate-to-high levels of poverty, 35% to 46% are also poor throughout early and middle adulthood. [19]
References
- ↑ Hall, L. (Jan. 12, 2021). “A Closer Look at Who Benefits from SNAP: State-by-State Fact Sheets”. Center on Budget and Policy Priorities.
- ↑ 2.0 2.1 (Sept. 01, 2020).“A Quick Guide to SNAP Eligibility and Benefits”. Center on Budget and Policy Priorities.
- ↑ 3.0 3.1 3.2 (March 3, 2021). Supplemental Nutrition Assistance Program: Students. United States Department of Agriculture.
- ↑ (October 28, 2020). Deciding To Go Out. United States Centers for Disease Control and Prevention.
- ↑ 5.0 5.1 5.2 5.3 Gingold, Naomi. (April 30, 2020).“Coronavirus Pandemic Complicates Getting Groceries with SNAP”. NPR.
- ↑ 6.0 6.1 6.2 Vasel, Kathryn. (May 30, 2018). “Too poor to afford food, too rich to qualify for help”. CNN Business.
- ↑ Dickinson, Maggie. (December 10, 2019). The Ripple Effects of Taking SNAP Benefits From One Person. The Atlantic.
- ↑ Eubanks, V. (2017). Chapter 1 From Poorhouse to database. In Automating Inequality. NY: St. Martin’s Press.
- ↑ 9.0 9.1 O’Neil, C. (2016). Introduction. In Weapons of Math Destruction: How Big Data Increases Inequality and Threatens Democracy. New York: Crown Publishing Group.
- ↑ 10.0 10.1 Obermeyer, Z., Powers, B., Vogeli, C., & Mullainathan, S. (2019, October 25). “Dissecting racial bias in an algorithm used to manage the health of populations.”. ScienceMag.org.
- ↑ (July, 2020).Official USDA Food Plans: Cost of Food at Home at Four Levels, U.S. Average, June 2020 1. United States Department of Agriculture.
- ↑ 12.0 12.1 Rao, Mayuree, et. al. "Do healthier foods and diet patterns cost more than less healthy options? A systematic review and meta-analysis". BMJ Journals, Accessed March 11, 2021.
- ↑ 13.0 13.1 Davis, G., You, W. (April 2020). The Thrifty Food Plan Is Not Thrifty When Labor Cost Is Considered, The Journal of Nutrition, Volume 140, Issue 4, April 2010, Pages 854–857
- ↑ Gupta, R. P., de Wit, M. L., & McKeown, D. (2007). The impact of poverty on the current and future health status of children. Pediatrics & child health, 12(8), 667–672. https://doi.org/10.1093/pch/12.8.667
- ↑ Berkowitz SA, Basu S, Gundersen C, Seligman HK. [State-Level and County-Level Estimates of Health Care Costs Associated with Food Insecurity. Prev Chronic Dis 2019;16:180549. DOI: http://dx.doi.org/10.5888/pcd16.180549
- ↑ Berkowitz, S., Seligman, H., Meigs, J., & Basu, S. (2018, September 10). “Food insecurity, healthcare utilization, and high cost: A longitudinal cohort study”.
- ↑ (Nov. 12, 2020).“Emergency room vs. urgent care: Differences, costs & options”. Debt.org.
- ↑ Sonik, R. A. (2019). “Health insurance and FOOD Insecurity: Sparking a Potential virtuous cycle”. American Journal of Public Health, 109(9), 1163-1165. doi:10.2105/ajph.2019.305252
- ↑ Wagmiller, R., & Adelman, R. (2009, November).“Childhood and intergenerational poverty: The long-term consequences of growing up poor”. National Center for Children in Poverty.